Fast Healthcare Interoperability Resources (FHIR) is a trending topic on the clinical side of the healthcare industry and is recognized as part of the solution to many of today’s escalating healthcare challenges. Healthcare providers have begun to adopt the open-source standard to improve interoperability, increase efficiency, and provide better patient care, among many other reasons. On the payer side of the healthcare industry, FHIR has faced a much slower adoption. However, payers stand to benefit significantly from adopting the standard as it enables easier integration with key partners, easier data exchange and interoperability across the payers healthcare ecosystem.
The Limitations and Interoperability Challenges of X12
Interoperability has become an increasingly pressing concern in healthcare, as the need to integrate data from multiple systems and sources has grown over the years. In the past, interoperability began with hospitals only needing to integrate a few systems within their walls. However, today’s hospitals have over 80 systems to consolidate, and the challenge is further compounded by the need to interoperate across many different hospitals. Today, with data coming from pharmacies, payers, labs, mobile devices, and other sources, the need for interoperability has evolved beyond integrating just a few systems.
The same is true for healthcare payers. The industry is becoming increasingly complex as providers consolidate, new alternative payment methods are introduced, and technology advances enable alternative care delivery settings such as digital health, remote patient monitoring devices and even hospital at home models. Payers need to leverage new, innovative models to be competitive, but their ability to connect with each of their partners on an EDI driven, point-to-point basis becomes less tenable as the total number of partners in their ecosystem continues to increase.
There’s more data, coming from an increasing number of sources, and stakeholders- including payers- that require access to it to make critical decisions. Those decisions have also grown more complex over the years. According to William Stead, Professor of Medicine at Vanderbilt University, in the past, there were only about 10 facts per decision in healthcare. Today, there are about 1,000 facts per decision, and the number continues to grow.

X12 has several drawbacks which prevent it from delivering the kind of interoperability required to see the bigger picture and make those decisions with confidence:
- X12 is a document exchange standard, but it’s not a data model.
- There’s no extensibility support, and the data model is very strict and rigid.
- There’s inconsistent use and enforcement of the rules, leading to a lack of standardization across entities.
- The rigid standard requires translation between different systems, adding complexity and time to data exchange.
- The standard is designed only for document exchange, making it inflexible and unsuitable for many modern use cases in healthcare.
X12’s limitations make it difficult for payers to gain a comprehensive understanding of their opportunities to control costs. Moreover, addressing the interoperability challenges of the X12 standard can be extremely costly and time-consuming, requiring significant investments in point solutions, as well as additional resources to increase its interoperability. In many ways, the healthcare industry has outgrown the capabilities of X12, and this trend will only continue to accelerate over time.
What Can Payers Achieve with FHIR?
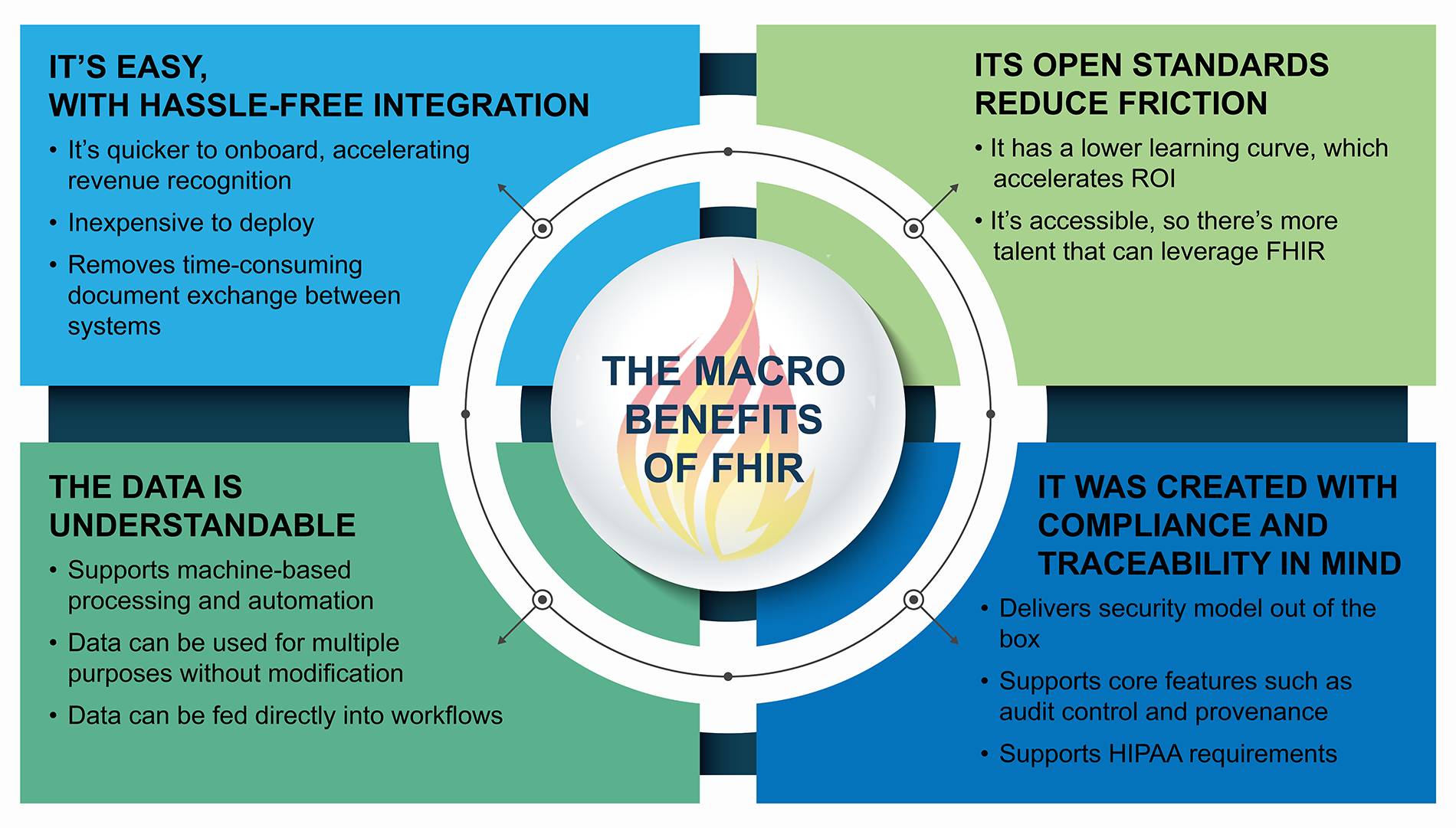
FHIR, the open-source standard for exchanging healthcare information, is not only beneficial for clinical applications but also has significant financial implications for payers. Payers can leverage FHIR to improve the quality of care and reduce costs by making their data accessible, interoperable, and standardized.
One of the key benefits of FHIR is its ability to capture and exchange more data from various sources. Payers can then use this data to make informed decisions about their networks and services, ultimately reducing costs. Additionally, FHIR’s flexible data model allows payers to tailor the standard to their unique workflows and data requirements, streamlining administrative tasks such as claims processing, enrollment, and network selection.
Ultimately, with the bigger picture of your data and less strain on resources due to the interoperability FHIR offers, payers are able to use the time and insight gained to find opportunities for cost-savings.
How FHIR Powers Intelligent Health Markets
By making healthcare data more accessible and interoperable, FHIR seamlessly enables Intelligent Health Markets.
An Intelligent Health Market brings the power of a marketplace to healthcare. It enables healthcare payers to connect to their entire ecosystem of preferred partners through a single connection, performing seamless data and operational exchanges with multiple partners. This provides the flexibility to integrate with best-in-class service providers, drive down the cost of integration and deliver it on a much faster timeline.
In an Intelligent Health Market, payers are able to proactively identify additional savings opportunities and leverage those savings to fuel innovation and growth within their healthcare system. Altogether, it becomes easier to provide your member populations with better quality and better prices, while increasing performance within your healthcare system and conserving its resources.
FHIR powers this experience by making the data accessible and actionable in a way that X12 can’t. By leveraging FHIR, payers can improve the quality of care, reduce costs, and fuel innovation and growth within their healthcare ecosystem. MacroHealth makes it easy to get started, providing solutions that dramatically reduce costs and increase performance within your organization while conserving its resources.
Contact us to speak to one of our experts today.
—
Sign up for the MacroHealth newsletter to learn more about how MacroHealth’s platform can help you overcome the challenges affecting healthcare business leaders today.
